DEFINITION OF CORONARY CIRCULATION
The blood and nutrition supply to the heart muscles (especially the myocardium) is called coronary circulation.
What is coronary circulation?
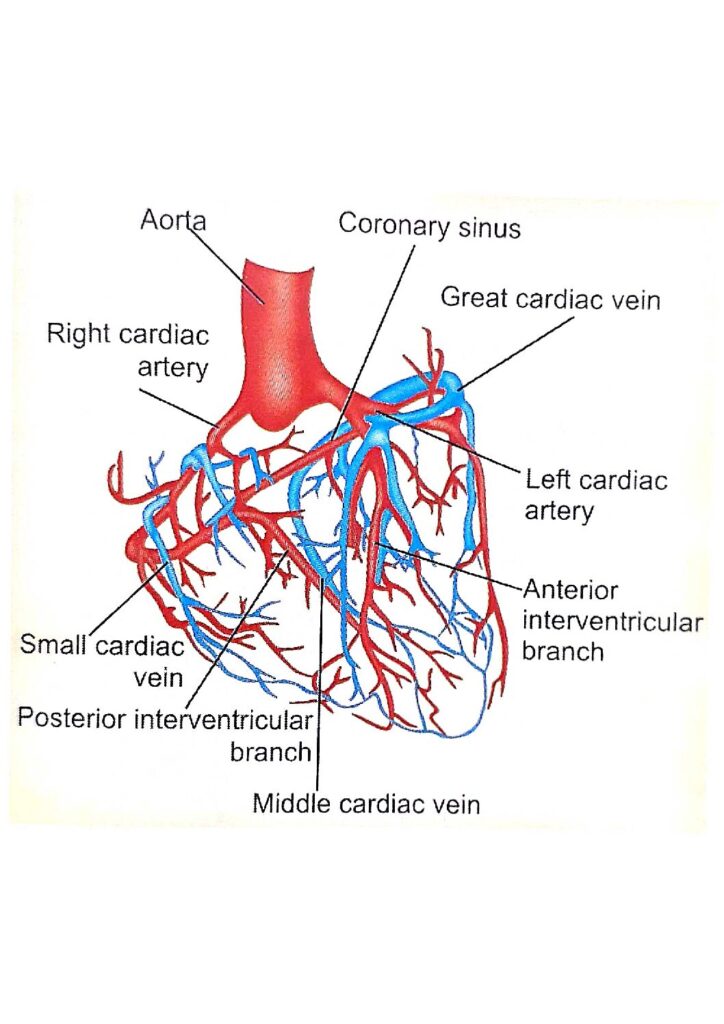
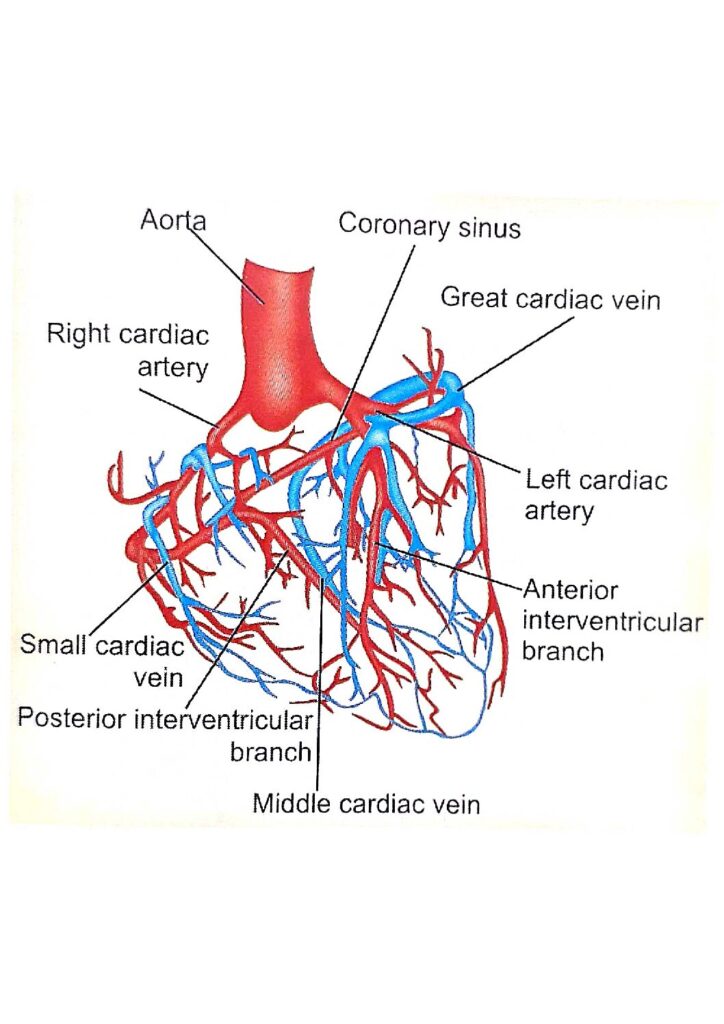
The two arteries supplying the heart, the right and left coronary arteries arise from the aorta above the aortic valve. The right coronary artery supplies the right atrium, right ventricle, and posterior aspect of the interventricular septum and the heart’s conducting system except for the left bundle of the conducting system. The left coronary artery supplies the left atrium left ventricle, and rest of the interventricular septum, and the left pile of the conducting system.
The coronary arteries divide and subdivide into smaller branches, which run all along the surface of the heart. The smaller branches also called epicardiac arteries give rise to final or intramural arteries which run at a right angle through the heart muscle near the inner aspect of the wall of the heart.
VENOUS DRAINAGE IN CARDIAC CIRCULATION
Three types of veins carry the venous drainage-
- The coronary sinus– 75% of the venous blood is collected into several small veins that join to form the coronary sinus, which opens into the right atrium. The remainder passes directly into the heart chambers through little venous channels.
- Anterior coronary veins– drain most of the right side of the heart and open directly into the right atrium.
- Thebesian veins– draining the myocardium open directly into the concerned chambers of the heart.
Read more: UNDERSTANDING OF THE RHEUMATIC HEART DISEASE
THE NORMAL BLOOD FLOW IN CORONARY CIRCULATION THE HEART: ANATOMY, STRUCTURE, AND BLOOD SUPPLY
- The normal blood flow through coronary circulation is about 200 ml/min. This blood flow is not constant. The flow decreases during systole due to compression caused by the contraction of the cardiac muscles. The flow is maximum during diastole when the condensation is released.
- 4% of cardiac output
- 65-70 ml/min/100g of cardiac muscle
What is a phasic flow
The blood flow through coronary arteries diminished during systole and increased during diastole, which is called phasic flow.
- The intramural vessels or final arteries supplying the myocardium are perpendicular to cardiac muscle.
- During contraction, the intramural vessels are compressed, and the flow of blood is reduced.
- The compression is released during diastole, and the blood vessels are distended. So blood flow increased.
Special features of the coronary circulation.
- The heart is the only organ of the body that generates its perfusion pressure.
- It is the organ in which the flow is reduced during systole.
- Coronary arteries are the end arteries and do not show proper anastomosis. Hence, a decrease in blood flow in one artery is not compensated by the other arteries.
- The rising atriovenous difference in o2 content is very high and extra demand for o2 during exercise is met by increased arterial blood flow.
- Metabolic factors like hypoxia are more powerful than neurological factors and coronary blood flow regulation.
- Capillary density per square millimeters is relatively higher.
Factors involved in coronary circulation
The coronary circulation is under auto-regulation of the heart and the factors involved in the regulation of the coronary circulation are:
1- Oxygen demand
It is the most important factor to maintain blood flow through the coronaries which is directly proportional to the oxygen consumption of the cardiac muscles. About 70 to 80% of oxygen in the blood is consumed by the heart muscles even at rest and this demand is enormously raised during increased cardiac activities like exercise.
2- Physical factors
- Arterial BP: coronary blood flow is directly proportional to BP, especially diastolic BP which increases the blood flow to the heart during diastole.
- Coronary vascular resistance: It mainly depends upon the viscosity of blood, diameter, elasticity of the coronary arteries, and velocity of blood flow.
- Myocardial compression: It decreases the flow during the systole increases the flow during the diastole, and increases the flow during diastole, and thus is responsible for phasic flow in the coronary circulation.
3- Chemical factors
- Hypoxia: It is a potent vasodilator of the coronary vessels which increases the coronary blood flow by coronary vasodilation through its direct effect and by action mediated through adenosine.
- Hypercapnia and acidosis: These factors potentiate the effect of hypoxia on vasodilation.
4- Coronary perfusion pressure:
It is the balance between mean arterial pressure and the resistance offered to the blood flow in the heart.
4- Neural factors
Coronary vessels are supplied by both sympathetic and parasympathetic nerve fibers. Stimulation of sympathetic fibers causes vasodilatation through receptors and vasoconstriction through receptors, the overall effect is vasodilation and an increase in the blood flow. Stimulation of the parasympathetic produces vasodilation and increased flow through direct impact and decline in blood flow through indirect effect.
5- Hormonal factors
- Catecholamines- Vasodilatation and increased coronary flow.
- Acetylcholine- Vasodilatation and increased coronary flow
- Vasopressin- Vasoconstriction and decreased blood flow.
- Angiotensin- Vasoconstriction and decreased blood flow.
- Thyroxine →increased blood flow →relative →hypoxia →vasodilation →increased coronary blood flow.
6- Role of cardiac output
Coronary flow is directly proportional to cardiac output. The coronary flow is increased by raising the aortic pressure.
7- Heart rate UNDERSTANDING OF BLOOD PRESSURE: TYPES AND TREATMENTS
Heart rate enriches the minute flow by decreasing the resistance of the capillaries.
8- Muscular exercise and excitement
Those two increase the coronary blood flow, enormously to meet the extra demand for oxygen by the cardiac muscles.
9- Anemia
In anemia, the coronary blood flow is enhanced to maintain the standard o2 needed for cardiac muscle.
Summary
The heart is supplied with two arteries. The right and left coronary arteries, branch from the aorta immediately distal to the aortic valve. The coronary arteries receive about 5% of the blood pumped from the heart, although the heart comprises a small proportion of body weight. The coronary arteries traverse the heart, forming a vast network of capillaries.
The heart receives blood through coronary circulation, to ensure a good supply of oxygen and nutrients.
References
M. Chendrasekar MD DA phD. Exam-oriented review in physiology. pp 216-18
FAQ
Q. (1)- What are the types of coronary circulation?
Ans- The great cardiac vein, the middle cardiac vein, small cardiac veins, and anterior cardiac veins are included in in coronary coronary circulation.
Q. (2)- What are 3 types of circulation?
Ans– Although the circulation of blood around the is continuous, it is convenient to describe it into 3 parts
- Pulmonary circulation
- Systemic circulation
- Coronary circulation
Q. (3)- What are the 4 main coronary arteries?
Ans– There are two main coronary arteries supplying blood to the heart. Then the coronary arteries divide and subdivide into smaller branches.
- Right coronary artery
- Left coronary artery
- Epicardial arteries
- Intramural arteries
Q. (4)- Which is the largest artery?
Ans– The aorta‘ is the largest artery in the body.
Q. (5)- Which is the organ of circulation?
Ans– The heart is the only organ of the body that generates its perfusion pressure.
Q. (6)- What are the two major arteries of the heart?
The right and left coronary arteries are major arteries of the heart.
Q. (7)- Which is the largest vein?
Ans– The superior vena cava and inferior vena cava are the largest veins in the body.
